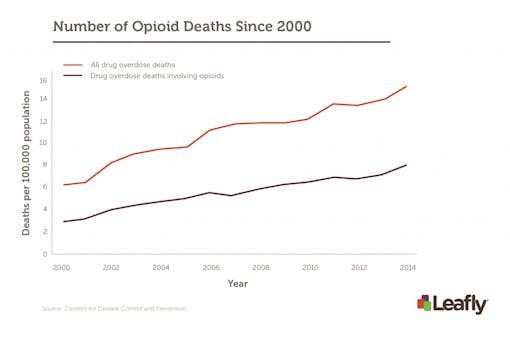
Those fortunate enough to only know the word “opioid” outside the context of personal tragedy may not realize what this addiction looks like up close. Opioid abuse is a scary-sounding statistic, with something to the tune of 19,000 Americans dying of overdose in 2014 alone, and a four-fold increase in opioid prescriptions written since 1999.
But for Stephen Mandile, an army veteran who served in the U.S. military for seven years before injury dismissed him, opioids represent a decade of struggle with pain – the kind of physical and emotional pain that has you leaning against the fence between life and death, wondering what could possibly be worse than an existence that seems a mockery of the word “life.”
“I was getting about two hours of sleep every few days, not caring about anything except for my next dose,” Mandile said. “Counting my pills all day to make sure I had enough of everything else for when my fentanyl would wear off, and I would go into withdrawal. I just wanted to die.”
In 2012, Mandile received a medical cannabis authorization in Massachusetts and waited three years for dispensaries to open their doors. “I was amazed at the pain relief I got from cannabis,” he recalled. “It helped with my migraines, my anger, my depression and my anxiousness. Within five months, I was finished with most of my VA meds.”

Number of opioid prescriptions by state. Some states have more prescriptions than people. (Click to enlarge.)
In 2014, a study found that states with medical marijuana laws saw 25% fewer deaths from opioid overdose compared to states without. Is this a mere correlation, or could there be more stories like Stephen’s that demonstrate how cannabis can help reduce opioid dependence? What’s most fascinating about this link, however, isn’t just that cannabis can substitute for opioids by virtue of its own analgesic properties. Studies are showing that one of its non-intoxicating constituents, cannabidiol (CBD), may actually treat symptoms of addiction.
The Story of Stephen Mandile

Stephen Mandile served in the U.S. military for seven years until he was injured in a motor collision.
“My time in Iraq is hard to describe,” Mandile began, recalling his time as a sergeant in the National Guard. “I felt honored to be around some great people, and proud to be serving America.”
Having ranked at the top of the civil service test in Massachusetts for police and firefighting, Mandile had a bright future ahead of him. But in 2005, a motor collision in Baghdad left him with five ruptured discs, sciatic pain, a narrowing spine, degenerative disc disease, spinal arthritis, lumbar radiculopathy in both legs and feet, traumatic brain injury, and major depressive disorder.
“[I was told] that I would end up in a wheelchair before I was 50 years old,” Mandile said, “So at 28 years old, I was left to figure out a new plan, but that never happened because of the lack of care, and an abundance of opioids.”
Awaiting his medical discharge at the “Wounded Warrior Unit,” with an expected wait time of 18 to 24 months, Mandile soon left, opting for an Honorable Discharge instead. “After a few days of seeing guys getting drunk, trading and overdosing on pills every night, and suicide attempts, I decided I needed to get out of there.”
Over the years, the VA would prescribe Mandile 57 different drugs for pain and depression: nine opioids including morphine, fentanyl, Vicodin, codeine, Percocet, oxycodone, and methadone; seven different muscle relaxants; six benzodiazepines including Xanax and Valium; seven antidepressants; and many others.
“I was a zombie.” Mandile said. “Five years of fentanyl left me with no desires of any kind. I was angry and depressed, with a temper and mood swings that put my wife through hell. But she always took care of me no matter what. I wished for death so I would stop burdening her.”
“After choking on a handful of oxycodone and fentanyl, it triggered something in me that made me realize I’m not taking these drugs, these drugs are taking me,” Mandile said. “Taking me to the grave if I kept doing it.”
That’s when Mandile took to the Massachusetts Statehouse to change the laws that nearly cost him his life.
Opioid Addiction Examined

This collection of pill bottles is symbolic of the many medications senior adults and chronically ill people take.
The reason why addiction is so hard to kick is the cyclic nature by which its symptoms occur. Opioids produce pleasure and euphoria, activating the brain’s reward pathways. With continued use, sensitivity to the drug decreases and more is required to achieve the same effect. At a certain point, cessation of the drug gives rise to withdrawal symptoms, or adverse effects like pain and anxiety. This encourages re-administration, leading to relapse.
The grip of opioids is particularly strong as they induce intense withdrawal symptoms – pain, nausea, vomiting, anxiety – while tolerance builds quickly. Opioid addiction is also characterized by particularly high relapse rates.
Cannabis has long been associated with its predominant psychoactive component, THC, but the second most abundant molecule, CBD, is taking center stage as a compound of immense clinical potential. Best known for its therapeutic benefits in pediatric epilepsy, CBD is now demonstrating its utility in treating addiction.
Most people tend to think of opioid addiction as occurring at the level of opioid receptors in the brain. However, multiple neurological systems are involved – systems that CBD also interacts with.
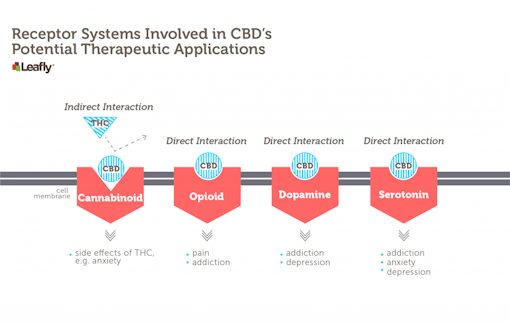
CBD interacts, either directly or indirectly, with many different receptor systems in the brain, a subset of which are shown here. For the treatment of addiction, CBD’s influence on serotonin receptors is the best studied. (Click to enlarge.)
Addiction, CBD, and the Brain

Active receptor isolated on blue.
We learn by association. The brain attaches meaning to otherwise meaningless aspects of our experience. Just as Pavlov’s dogs learned to salivate at the sound of a bell indicating food was coming, people create strong associations from good and bad experiences. For example, a sound or smell might trigger a traumatic memory in a PTSD patient. A place or friend might trigger an urge to drink in a recovering alcoholic. These types of triggers – technically known as “cue-induced cravings” – are often the cause of relapse.
Scientists have found that CBD can help dissolve these associations through interactions with the serotonin system. Serotonin is a neurotransmitter commonly associated with mood, but it also plays a role in addiction. Preclinical research shows that CBD can reduce drug-seeking behavior, diminish withdrawal symptoms, and limit cravings.
A common way neuroscientists study addiction is to set up an experiment where a rat is trained to press a lever to receive a reward. The reward can be a drug like morphine or an electrical zap into one of the brain’s pleasure centers. Rats will do lots of lever-pressing for big rewards, but when researchers add CBD to their systems, rats don’t do as much.
Drugs of abuse like morphine are said to be “reward-facilitating” because they make animals work harder than they otherwise would for zaps to their pleasure center. For example, a rat might press a lever five times in a given period, receiving five zaps of pleasure from a stimulator in its brain. If you give that rat morphine, it will press the lever even more. Thus, drugs like morphine make animals even more sensitive to rewards than they are naturally.
Giving rats CBD actually blocks this effect of morphine. On its own, a rat might work for five zaps of pleasure. With morphine in its system, it might work for ten. But if you give it CBD before giving it morphine, it will work for five, like it did with no drugs in its system.
CBD’s interaction with the serotonin system is critical for its ability to block morphine’s effects on reward-seeking behavior. If a specific serotonin receptor is blocked, CBD no longer has this effect. Since we know that CBD can directly stimulate serotonin receptors, this means that its ability to help treat addiction likely depends on its actions at serotonin receptors.
“Currently most medications for opioid abuse directly target the endogenous opioid system,” researchers have written, weighing the clinical importance of such findings. “CBD could thus offer a novel line of research medication… helping to reduce side effects normally associated with current opioid substitution treatment strategies.”
CBD in Human Clinical Studies

A scientist examines a sample in a modern laboratory.
Building on animal research, pilot studies in humans have been conducted. At this stage, researchers evaluate the safety and side effects of treatments. In a double-blind, placebo-controlled phase I trial, CBD co-administered with fentanyl was well-tolerated and had no adverse effects. Once a drug’s safety profile has been established, it can be tested in larger groups.
Next, a small study was conducted to investigate CBD’s effects on drug cravings in heroin-dependent individuals. Basically, they gave heroin addicts a dose of CBD or placebo on three consecutive days. They then showed them opioid-related or neutral video cues and measured cue-induced drug craving. They did this one hour, one day, and one week after CBD/placebo administration. CBD decreased cravings and anxiety at all time points.
In other words, these small pilot studies in humans are consistent with animal research showing that CBD can diminish cravings and anxiety triggered by drug-associated cues. This is key, because drug relapse in recovering addicts often follows exposure to such cues. A therapy that diminishes an addict’s response to these triggers is what we desperately need.
The potential CBD has shown is remarkable, and it’s no coincidence that fentanyl manufacturer Insys is running clinical trials on CBD while simultaneously funding anti-legalization efforts in its home state of Arizona.
Ending the Opioid Epidemic

Marijuana buds organized into a weekly pill case.
It’s difficult to untangle from our national consciousness the negative messages emitted by anti-drug campaigns over the years. Nonetheless, public approval of cannabis legalization has never been higher. Part of the reason for this comes from research that has disproved time and time again that cannabis is not what the failed War on Drugs describes.
But there’s another reason for cannabis legalization – one that speaks to the stories of veterans, parents, and patients who have found hope in cannabis. For Stephen Mandile, the fight for legalization continues.
“My young daughters definitely prefer Daddy now, compared to Daddy on opioids and pills,” Mandile said. “Cannabis allowed me to ignore the pain and withdrawals of fentanyl, oxycodone, and Xanax. Without cannabis, I’m sure I would have overdosed or committed suicide by now.”
“In June, I was forced to go back on fentanyl because I could not afford cannabis or birthday presents for my daughters,” he continued. “I begged the VA to give me medical cannabis instead.”
When Mandile had an opportunity to speak with Massachusetts’ Governor Baker, he shared his story and asked for help in addressing the problems with veteran care. “I told him we need to stop the opioid epidemic and stop the 22 veterans suicide that occur every day, many of which occur by opioid overdose. He agreed to talk with me because he believed they were serious issues, yet I still haven’t heard from him.”
Never standing down, Mandile spent several days and nights outside the Statehouse attempting to reach the lawmakers who could help him achieve reform. He’s also started a non-profit charity – Veterans Alternative Healing – to help veterans with opioid addiction through a variety of different therapeutic options.
Legalization and the Hope of Change

Photo credit: Ed Schipul/Flickr Creative Commons
United States drug policies are the vehicle by which the opioid epidemic was injected into America. Legal painkillers are killing our loved ones by the tens of thousands. Many more live pill-to-pill, trying desperately to extinguish the very pain that those pills were prescribed to treat.
Meanwhile, the only destroyed lives attributable to cannabis are those caused by the War on Drugs itself: the bodies left in the wake of black market drug operations; the children with epilepsy who, without CBD, are left comatose by their prescription medications; the Americans who spend their lives in prison at disproportionate rates based on race; the countless other people dedicating their lives to fight for a world made better by this plant.
When you’re looking at the November ballot, wondering whether or not to legalize cannabis, know that this is not only a battle many fight for freedom, but for life itself.